Shifting from the current fee-for-service, quantity-based healthcare model to a value-based care model (VBC) has not been easy for providers. Leading the charge towards VBC is the Centers for Medicare and Medicaid Services (CMS) who, along with Health Care Payment Learning & Action Network (HCPLAN), is expecting 100% of provider reimbursements to be tied to value-based contracts by 2025. The intent in this new healthcare model is to reward higher quality of care to patients while reducing costs. With this inevitable healthcare model shift, providers should understand the challenges they may face during their transition.
What is Value-Based Care?
Value-Based Care is a healthcare delivery model where providers – including hospitals, doctors, nurses, and labs – receive pay based on the quality of care they give, not the quantity. Providers would no longer be paid separately for each medical service rendered. To do this, payers and providers will not only share in financial risk through Accountable Care Organizations (ACOs), but VBC programs will offer additional incentives designed around quality care measurements, including the health outcomes of their patients.
Providing healthcare in a quantity-based world can’t continue; healthcare spending has reached astronomical levels and offers little value to patients. In fact, the US spends the most on healthcare while also having the highest disease burden compared to other high-income, developed countries. In 2020, CMS revealed that US healthcare spending grew 9.7%, reaching $4.1 trillion – that’s $12,530 per person – and accounted for 19.7% of Gross Domestic Product. They also projected that healthcare spending will reach $6.2 trillion by 2028.
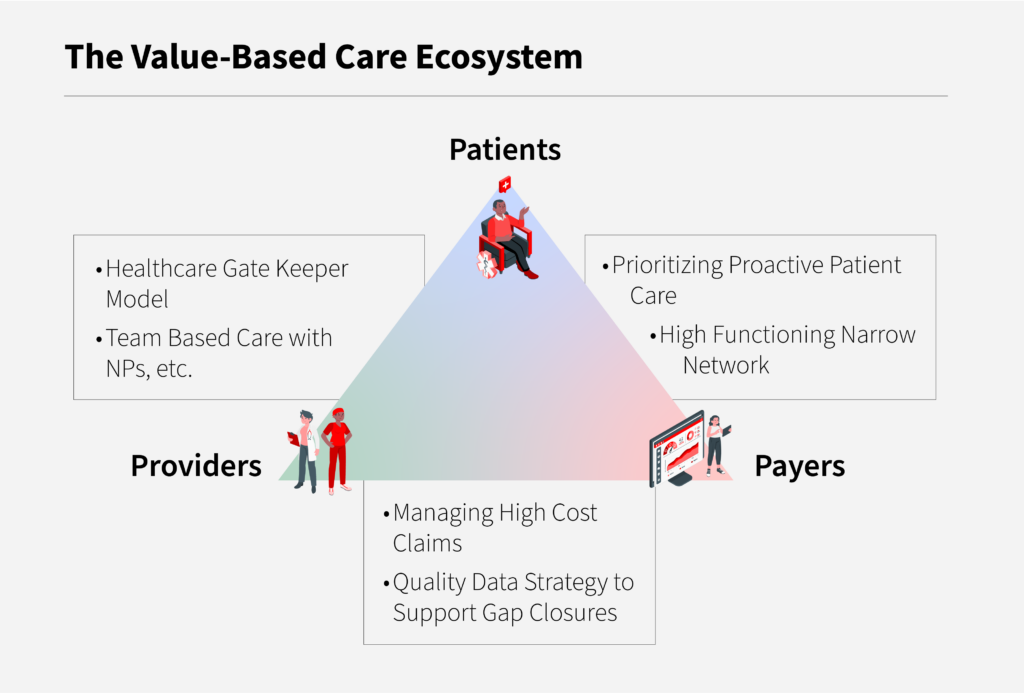
In order to improve the value of care, we need a model that improves care quality and reduces cost: value = quality/cost equation. With VBC’s triple aim – improve healthcare experiences, improve patient’s health, and reduce healthcare costs – this new model represents a critical step in the right direction by adopting a team-oriented, data-driven approach. The collaboration of payers, providers, and patients is essential in order to drive success with this model. Engaging patients towards total health is key, and something that is led by a primary care physician as well as supported by a multi-disciplinary care team; this avoids the patient having to navigate the healthcare system on their own.
4 Challenges in Shifting to a Value-Based Care Model
While VBC continues to transition into the provider’s main means of healthcare delivery, there are still major challenges and barriers impeding an easy shift. To accomplish a successful transition, it’s important for organizations and providers to understand the most common challenges in order to better prepare for and overcome them.
1. Unpredictable Revenue Streams for Providers
One of the biggest challenges in gap closure is provider buy-in. Seventeen percent of provider teams have fears about revenue stream and sustainability, and have difficulty understanding the financial risks when adopting to a VBC model and affiliated programs.
If you have a team that is not incentivized to participate in dual billing, or to see patients in a more proactive way, the extra effort is then seen as more work without compensation. Organizations need to design an effective structure for their practice to meet value-based goals, keeping their teams invested from both a quality and financial perspective.
2. Lack of Meaningful Data and Data Interoperability
A key component to a successful VBC strategy is having data integrity and easy, intuitive accessibility to data. Data interoperability continues to be one of the biggest challenges in shifting to a VBC model, according to 19.7% of providers. Data means nothing if it’s not presented and displayed in a digestible manner for the target audience. For example, there is a tremendous amount of data available from payers and providers through disparate systems and unstructured data by means of notes, images, etc. This leads to data paralysis and challenges the ability to gain meaningful insights at the right time – a key element in addressing gap in care within the VBC model.
Also, many value-based payment mechanisms rely on complex data, electronic health information, and sophisticated quality and performance measures. When payments become linked to quality, health outcomes, and provider performance, the payer must ensure the reliability of that underlying data. To ensure reliable results, the measures must be appropriate and meaningful, and the data must be accurate, complete, and timely. To facilitate and support the gathering of appropriate and meaningful data, it’s imperative to have effective systems in place – such as interoperable EHR systems, telehealth technologies, and core operational and financial applications – that complement your existing structure. And with AI technology evolving faster than ever, health systems must adopt these technologies to get real time, actionable, and meaningful data in order to take care of their members on time, to reduce the cost of care, and to improve patient engagement and satisfaction.
3. Outdated IT Systems
Though many healthcare practices have modern technologies implemented, there are still a large number of healthcare systems using outdated applications and core and claims management software. This can also link back to systemic issues regarding data integrity and reporting capabilities. Inefficient and outdated technology also creates a negative impact on the patient experience, leaving them to pursue another practice that offers more value. Implementing a new innovative platform can ensure the successful deployment for overall success in patient outcomes and experiences, as well as health system workflows.
4. Lack of Transparency and Effective Governance
The VBC model is all about sharing risks, costs, and incentives between payers and providers. Every payer and provider are different in their focus, culture, and measures of success; measurement of each metric and KPI, and their interpretation, can be perceived differently for each player. Building a joint governance model brings commitment and transparency and enables the ability to share feedback on success and areas of improvement on a regular basis. This creates long-term trust, better member engagement, and better delivery of care, which effectively results in a successful VBC delivery.
Divurgent Can Help
Breaking these barriers and overcoming these challenges demands a strong team of industry experts and IT professionals. Divurgent, with its offering of View Analytics, can address the IT implementation strategy and build robust systems for data exchange, actionable data insights through predictive data analytics, and KPI measurements, all while tying it back to care team compensation and various analytic models to reduce cost. With the right experts, the right technology, and the right approach, healthcare providers can overcome these challenges and meet their value-based goals while providing quality patient care.


