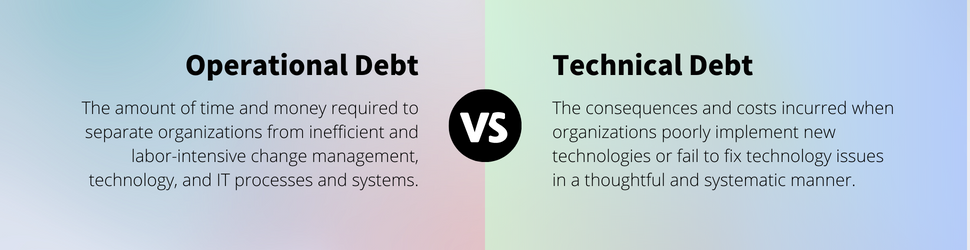
The interplay of operational debt and technology debt often produces a compounding snowball effect until your organization experiences an avalanche of inefficiency. Operational debt arises from suboptimal processes, decisions, and poorly implemented technology that leads to inefficiencies and waste, while technology debt arises from suboptimal technology choices, architecture decisions, or code quality issues.
This interplay and its impact on the stakeholders were recently witnessed with a large US-based grocery chain when a customer lost a receipt related to a work purchase. A visit to the store to obtain a copy of the receipt resulted in multiple phone calls to customer service, a mail-in form, and weeks of waiting for a copy of the transaction. “It’s 2023, and we are sending civilians to space,” the customer responded, “we must be able to do better than mailing a form.” After one store visit, a failed workaround attempt, three phone calls, and multiple weeks, they returned to square one and mailed the form. That’s when the customer wondered if the receipt could be living in the store’s mobile app – surely, out of habit, they used their loyalty card with the purchase. After a quick search in the mobile app, they found their receipt.
The wasted time and frustration experienced by the stakeholders could have been avoided if the operational debt didn’t exist. Two simple questions by the first staff member they encountered could have solved the problem. “Did you use our loyalty card to make the purchase? Do you have our app?” Boom, done, receipt found. What if the answer to these questions was no? Do the customer’s needs go unfulfilled?
In healthcare, sadly, this is not uncommon. Take online appointing for example. The digitally mature patient wants to make appointments online but are often confronted with barriers. They either begrudgingly make a phone call, don’t make that call at all, or worse yet, receive a phone call to reschedule. Whether the barrier is operational or technology related, efficiency on both sides is sacrificed which creates debt.
How to Address Operational Debt
In order to address operational debt in healthcare, organizations must take a holistic approach that considers technical and non-technical factors. Ultimately, this requires ongoing attention and investment in process improvement, technology modernization, and organizational culture. Healthcare organizations should leverage patient-facing and internal digital capabilities to stay competitive. They must improve communication channels, streamline the service delivery process, and set organizational goals to maximize these capabilities. Allowing the continuation of operational debt results in lost revenue, increased expenses, burnout, and both patient and staff dissatisfaction.
1. Improve Communication Channels
Healthcare organizations often turn a blind eye to unclear communication; thus, digital capacity suffers, and operational efficiency declines. Investing in human-centered communication can improve stakeholder engagement, reduce resistance to change, and enhance the overall success of change initiatives. This includes developing tailored, clear, concise, and relevant messages that are delivered through multiple channels to ensure that all stakeholders receive the necessary information.
Key activities include:
- Identify and engage stakeholders: In healthcare, it’s essential to identify all stakeholders who may be impacted by the change and engage them in the communication process. This includes patients, healthcare professionals, support staff, and management. Communication should be tailored to each stakeholder group’s needs and preferences to ensure that they receive the right information at the right time.
- Use multiple communication channels: Healthcare organizations should use a variety of communication channels to reach stakeholders effectively. This may include in-person meetings, emails, social media, newsletters, and intranet portals. Each communication channel should be carefully selected based on the audience and the message being delivered.
- Provide clear, concise, and consistent messaging: Healthcare organizations should ensure that the messaging around the change is clear, concise, and consistent. Communication should be jargon-free and avoid technical language that may confuse stakeholders. It’s also essential to provide regular updates throughout the change management process to keep stakeholders informed and engaged.
2. Use Service Blueprints
Take another example – after eCheck-in in for an appointment, the front-desk staff greeted the patient with the question, “Was everything correct when you checked in online?” Only months before, at the same office, using the same eCheck-in process, the same questions updated just 30 minutes prior were asked again. Yes, finally someone is getting it! They’re letting the technology work for them, allowing for a more personalized and pleasing experience. For a practice that easily sees more than 200 patients a day, check-in took less than 30 seconds, there were no lines, and customers were promptly greeted.
Digital capabilities can help healthcare organizations improve operational efficiency, reduce paperwork, and eliminate unnecessary tasks. By using service blueprints to outline all steps in a delivery process, healthcare organizations can identify inefficiencies and bottlenecks in their processes and develop strategies to eliminate them. Furthermore, decisions can be made regarding which processes should remain part of the human experience and element. Once the inefficiencies are identified, new human-centered design and automation processes can be implemented. Automating patient check-in, registration, or online appointing isn’t enough. True value for our patients and staff won’t be realized unless organizations address the operational debt associated with the implementation.
Key activities include:
- Identify the patient journey: Start by identifying the patient journey and mapping out the different stages of the experience, from pre-arrival to post-treatment. This will help you understand the touchpoints between patients, healthcare providers, and where opportunities for improvement exist.
- Engage with staff: Engage with staff members who work in different roles within the healthcare organization to identify any pain points or areas of inefficiency in the patient journey, technology, and tools. This will help ensure that the service blueprint is accurate and reflects the realities of the healthcare environment.
- Prioritize improvements: Once you have identified areas of opportunity for improvement and automation, prioritize which ones to focus on first. Start by identifying the pain points that are causing the most significant issues for patients and staff and develop a plan to address them. Additionally, account for and highlight current processes that add value, ensure you maintain or enhance the fidelity of these. As you make improvements, continue to monitor and update the service blueprint to ensure that it remains an accurate reflection of the patient journey.
When you apply these principles to the eCheck-in example, you’ve now ensured alignment between the digital and human touchpoints, and you’ve engaged the staff to help them understand that the patient’s journey started before they were greeted and added value to the interaction. Efficiency is improved!
3. Set Organizational Goals and Increase Visibility
To achieve their goals, healthcare organizations must establish organizational objectives, set measurable key performance indicators (KPIs), and ensure visibility across all departments. Dashboards can provide real-time data and metrics that allow healthcare organizations to track progress and make data-driven decisions. Dashboards can be customized to show performance data at the departmental, team, or individual level, allowing healthcare organizations to identify areas for improvement and action. Fostering a data-driven culture and empowering your front-line staff to understand how data can help improve their efficiency is paramount. Additionally, data can help inform future iterations of digital capabilities to assist staff with continued increases in efficiency.
Key activities include:
- Clarify priorities: Setting clear and measurable goals helps organizations to prioritize their efforts and allocate resources accordingly. By focusing on the most important goals, organizations can streamline their activities and optimize their digital capacity.
- Increase accountability: Goals provide a framework for measuring progress and evaluating success. By setting specific targets, organizations can hold themselves accountable for achieving results, take corrective actions if necessary, and celebrate iterative wins and improvements. This helps to ensure that the organization is on track to achieve its digital objectives.
- Improve communication and collaboration: When goals are clearly defined, it becomes easier for teams to understand their roles and responsibilities, and work together towards a common objective. This leads to improved communication, collaboration, and coordination, which can increase visibility and digital capacity within the organization.
Work with Divurgent to address your organization’s operational debt and chart a path forward.

About the Author

Kristal Wittmann | Director of Digital Health
Kristal is a detail-obsessed and tech-savvy professional with comprehensive experience in operational leadership and program management. She keeps a keen focus on technological advancements and process improvements within patient care and services sectors. Experienced in leading cross-functional technical and non-technical teams to design, develop, and manage automation and cloud implementation projects, she is well-versed in formulating effective strategies to drive overall program execution and process improvement initiatives. To learn more about Kristal, visit her LinkedIn.


